Member News
ASE Appoints 2025-2026 President
July 3, 2025
Announcements
2026 ASE Award Nominations Open
June 24, 2025
Member News
2025 Coding Connection
June 23, 2025
ASE News
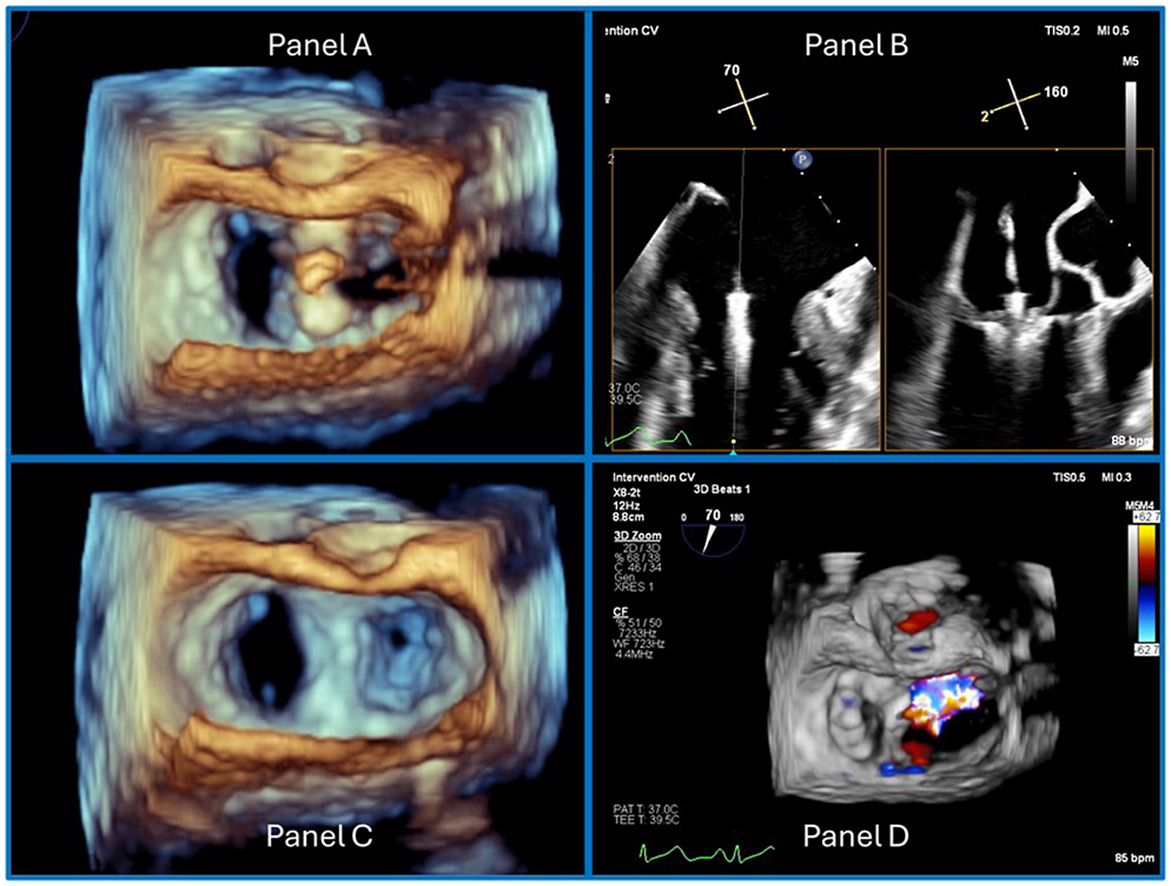
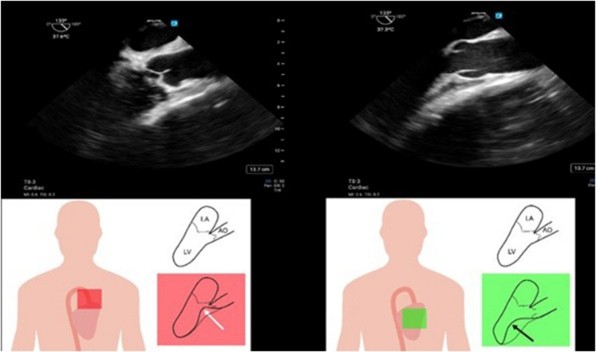
June CASE: Just Useful, Noteworthy Examples
June 17, 2025

Announcements
ASE and CRF® Launch New Educational Collaboration
June 12, 2025

Announcements
Remembering Roberto M. Lang, MD, FASE
June 11, 2025

Announcements
A Jam Packed June JASE
June 4, 2025
Announcements

Press Release
ASE Announces 2025-2026 Board of Directors
May 8, 2025
Announcements
May This JASE Issue Bring You New Insights
May 6, 2025
