The Centers for Medicare and Medicaid Services (CMS) is proposing significant changes to office and outpatient evaluation and management (E/M) codes that are expected to take effect January 1, 2021.
Current Procedural Terminology (CPT) codes 99201–99205 and 99211–99215 covering physician office-based services or physician services provided in the outpatient setting for new or established patients are the affected codes. The changes are intended to simplify administration, address payers perception that the current E/M codes as “outdated,” and increase the amount of time physicians spend caring for patients.
It is important to note that these changes also impact the payments for services that fall under the Medicare Physician Fee Schedule (PFS). CMS estimates that the changes to 2021 policies, including increased cost of E/M visits, will increase Medicare PFS spending by $10.2 billion. To comply with budget neutrality requirements, any payment increases must be offset by corresponding decreases. Therefore, CMS proposed the CY 2021 PFS conversion factor be reduced to $32.26, which is a decrease of $3.83 from the CY 2020 PFS conversion factor of $36.09. This change is required by law which states that any changes to the PFS cannot increase or decrease spending by more than $20 million.
What does this mean to you?
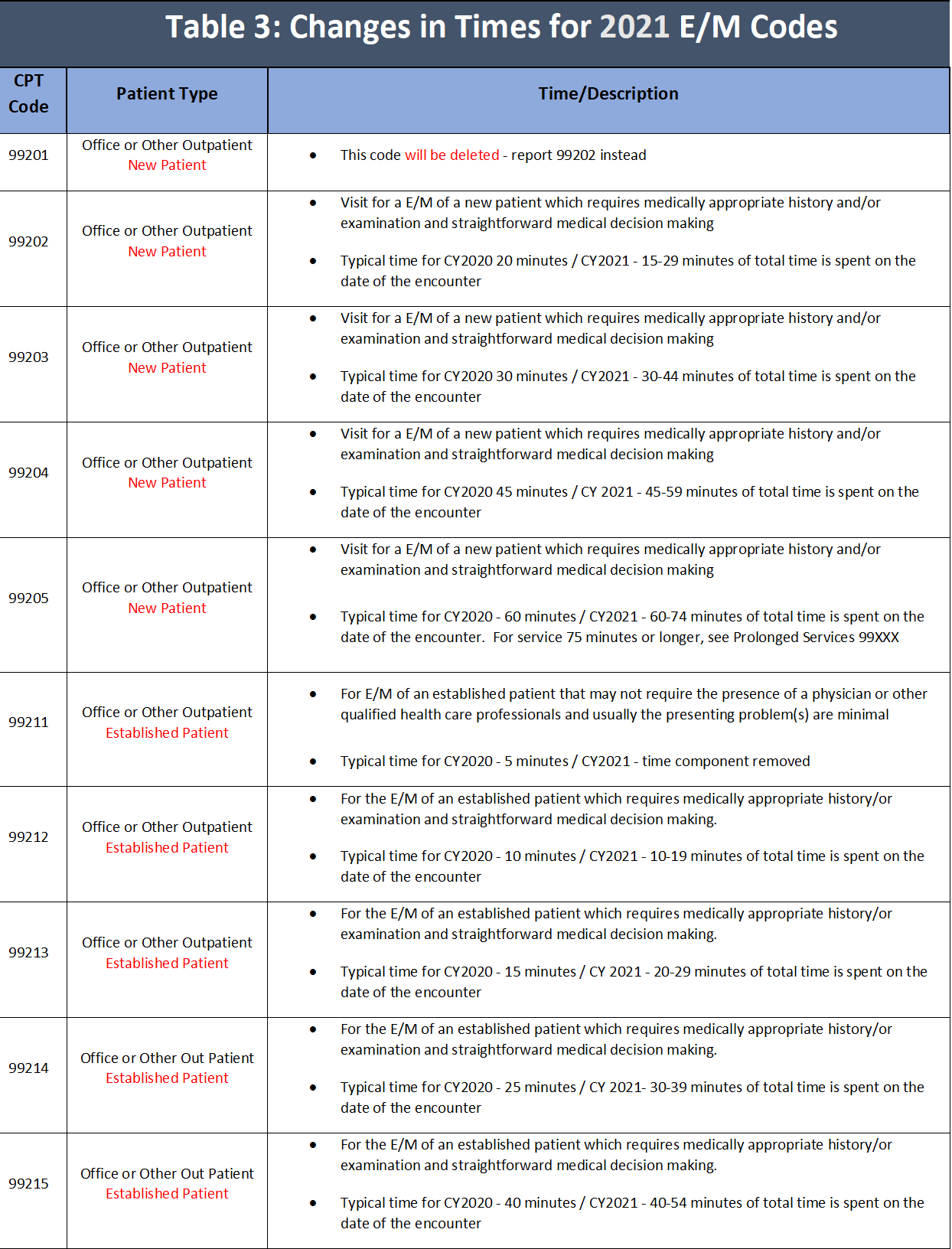
Beginning January 1, 2021, it will be important for you to bill your E/M level of service, for office or other outpatient services, based on either medical decision making (see Table 2) or time (see Table 3). Time will be counted as total time spent with patient on date of service (including non-face-to-face services). This is a change from current practice.
Key elements of the E/M office-visit overhaul include:
- Eliminating history and physical exam as elements for code selection. While significant to both visit time and medical decision-making, these elements alone should not determine a visit’s code level.
- Allowing physicians to choose whether their documentation is based on medical decision-making or total time. This builds on the movement to better recognize the work involved in non-face-to-face services like care coordination.
- Changing medical decision-making criteria to move away from simply adding up tasks to instead focus on tasks that affect the management of a patient’s condition.
The American Medical Association (AMA) has developed a detailed guide of the changes. Over the next several weeks, ASE will be supplementing this information with helpful tips specific to our membership to assist in preparing your practice to implement these changes.
The following tables provide an overview to lay the groundwork for understanding the coding changes. These include: Comparison to other E/M services (Table 1); Level of Medical Decision Making (Table 2) and changes in time for office and other outpatient services (Table 3).
In the near future ASE will provide details around each revised section and decode selection of appropriate E/M Level for both new and established patients. Additionally, we will provide information on prolonged services add-on codes; changes to other E/M related services, and tips and tricks for implementation for these January 1, 2021 changes.
Table 1: Overview of major E/M revisions for CY2021: Office and other outpatient services vs other E/M
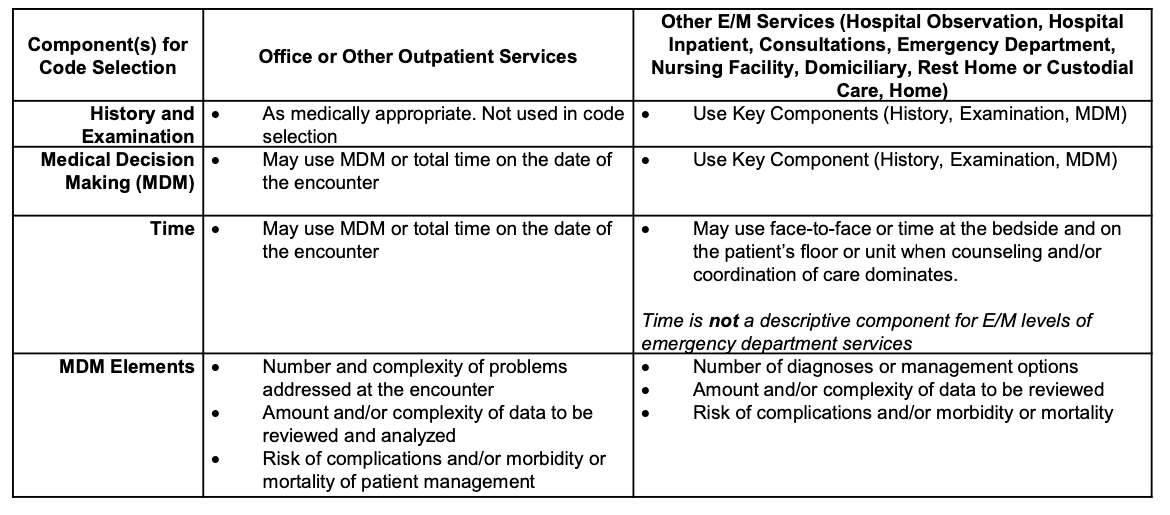
Source: https://www.ama-assn.org/system/files/2020-04/e-m-office-visit-changes.pdf
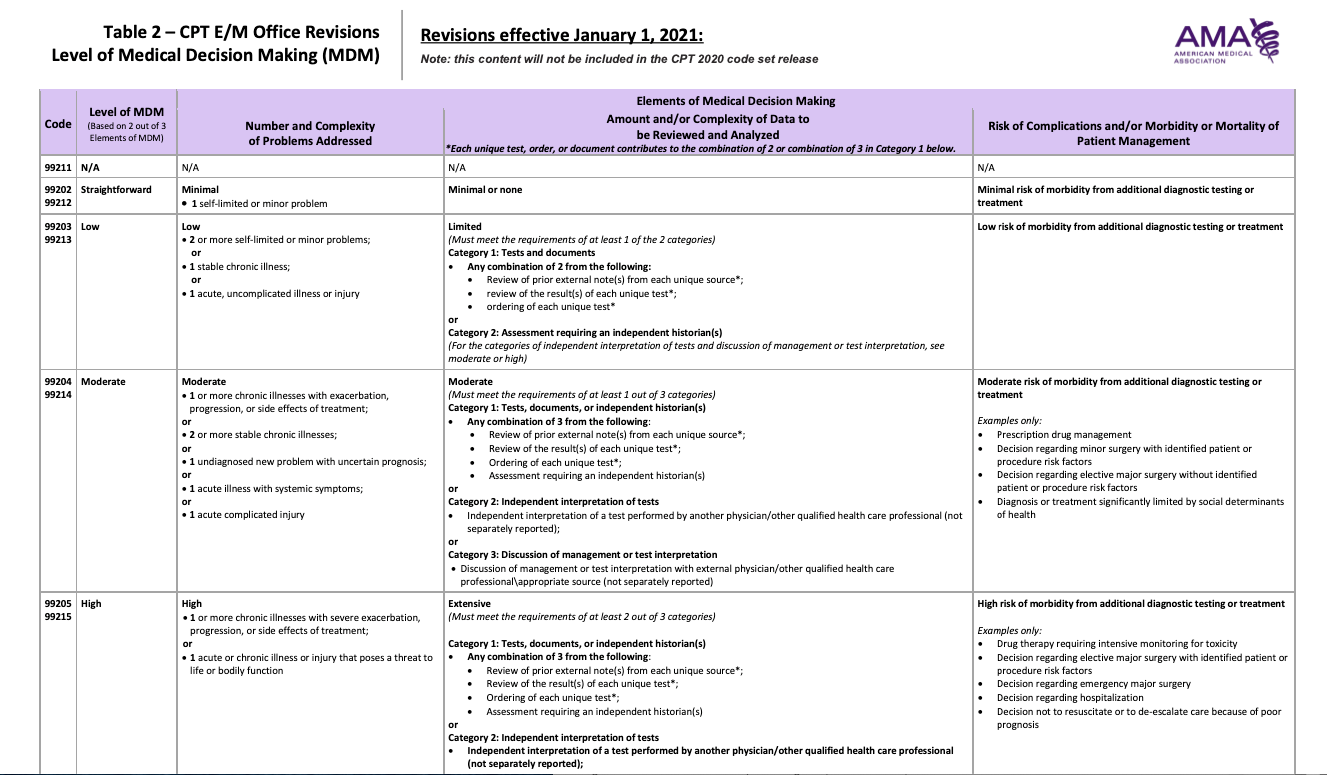
Source: https://www.ama-assn.org/system/files/2020-04/e-m-office-visit-changes.pdf