On July 7, 2022, the Centers for Medicare and Medicaid Services (CMS) released the CY 2023 proposed Medicare Physician Fee Schedule (MPFS) Rule. This proposed rule announces and solicits public comments on the proposed policy changes for Medicare payments under the Physician Fee Schedule (PFS), and other Medicare Part B issues, for services effective on or after January 1, 2023. Comments will be accepted until September 6, 2022.
Conversion Factor & Impact to Echocardiography
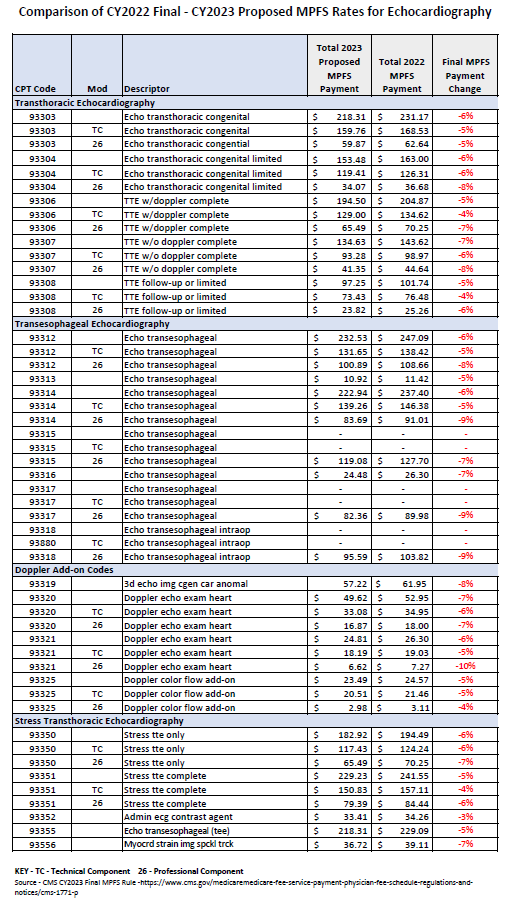
The proposed CY 2023 PFS conversion factor is $33.08, a decrease of $1.53 to the CY 2022 PFS conversion factor of $34.61. This conversion factor accounts for the statutorily required update to the conversion factor for CY 2023 of 0%, the expiration of the 3% increase in PFS payments for CY 2022 as required by the Protecting Medicare and American Farmers from Sequester Cuts Act, and the statutorily required budget neutrality adjustment to account for changes in Relative Value Units. As a reminder, CY 2023 is the second year of a four-year phase to practice expense changes. As noted for CY 2022, CMS updated the clinical labor portion of the practice expense inputs. These updates ultimately resulted in cuts to practice expense elements of echocardiography services.
Additionally, changes noted below to several evaluation and management (E/M) code families, including hospital, emergency medicine, nursing facility and home visits, as recommended by the CPT Editorial Panel and AMA/Specialty Society RVS Update Committee (RUC) are estimated to require an additional reduction of about 1.5% to the 2023 Medicare conversion factor due to statutory budget neutrality requirements. Finally, the impact table in the proposed rule does not seem to include the 3% reduction in the conversion factor.
Evaluation and Management (E/M) Visits
As part of the ongoing updates to E/M visits and related coding guidelines that are intended to reduce administrative burden, the AMA CPT Editorial Panel approved revised coding and updated guidelines for other E/M visits, effective January 1, 2023. CMS is proposing to adopt most of these changes in coding and documentation for other E/M visits (which include hospital inpatient, hospital observation, emergency department, nursing facility, home or residence services, and cognitive impairment assessment) effective January 1, 2023. CMS is also proposing to maintain the current billing policies that apply to the E/M visits while they consider potential revisions that might be necessary in future rulemaking.
Split (or Shared) E/M Visits
For CY 2023, CMS is proposing to delay the split (or shared) visits policy finalized in CY 2022 for the definition of substantive portion, as more than half of the total time, for one year with a few exceptions. Therefore, for CY 2023, as in CY 2022, the substantive portion of a visit may be met by any of the following elements – history; performing a physical exam; making a medical decision or spending time (more than half of the total time spent by the practitioner who bills the visit).
Under this proposal, clinicians who furnish split (or shared) visits will continue to have a choice of history, physical exam, or medical decision making, or more than half of the total practitioner time spent to define the substantive portion, instead of using total time to determine the substantive portion, until CY 2024.
Telehealth Services
For CY 2023, CMS is proposing a number of policies related to Medicare telehealth services including making several services that are temporarily available as telehealth services for the Public Health Emergency (PHE) available through CY 2023 on a Category III basis, which will allow more time for collection of data that could support their eventual inclusion as permanent additions to the Medicare telehealth services list. CMS is proposing to extend the duration of time that services are temporarily included on the telehealth services list during the PHE, but are not included on a Category I, II, or III basis for a period of 151 days following the end of the PHE, in alignment with the Consolidated Appropriations Act, 2022 (CAA, 2022). CMS is also proposing to implement the telehealth provisions in the CAA, 2022 via program instruction or other subregulatory guidance to ensure a smooth transition after the end of the PHE.
Proposed Payment Rates for Echocardiography Services
PFS fact sheet
Quality Payment Program fact sheet (link downloads a .zip file)
Medicare Shared Savings Program Proposals fact sheet
ASE is beginning our analysis of the Proposed Rule and will provide a summary analysis and fee schedule impacts for members promptly.